Can you be fat and still be fit? An estimated 15% to 20% of obese individuals have none of the metabolic derangements associated with obesity, such as high blood sugar, high blood fats, high blood pressure, Type 2 diabetes and other risk factors for cardiovascular disease.1
This phenomenon has led to the idea that you can be obese yet in good health. But according to recent research,2,3,4 this popular belief — known as “metabolically healthy obesity” (MHO) — is a fallacy. As reported by studyfinds.org:5
“The myth of being ‘fat but fit’ is, again, being debunked by a new study. Researchers found that obese individuals, even if they appear healthy, have an increased risk of diabetes and … are still 50% more susceptible to coronary heart disease.”
No Such Thing as ‘Fat and Fit’
According to professor Matthias Blüher, who presented the findings at the 2023 Meeting of the European Association for the Study of Diabetes,6 high body mass index (BMI) in combination with normal glucose and lipid levels, and the absence of high blood pressure, is not sufficient for MHO classification. Rather, it’s the behavior of the adipose cells that matters.
People who have normally sized adipocytes (cells that store fat), have far fewer obesity complications compared to those who have enlarged and inflamed adipocytes.
Dysfunctional adipocytes can result in fibrosis and the release of harmful molecules that contribute to organ damage. Fat-secreted hormones, known as adipokines, can also directly affect cells in your vascular system, leading to atherosclerosis.
Where you store most of your fat may also be key. Obese individuals with large visceral fat stores, meaning the fat is primarily stored around their internal organs, are far more likely to develop Type 2 diabetes than those whose fat stores are distributed more evenly around their body, the study found. Other studies have also confirmed this.7
What this means in practical terms is that obese patients still need to focus on losing weight and may need other preventive treatments as well. In an October 3, 2023, press release, Blüher explained:8
“So there is still a residual increased risk for those people living with obesity, even with what we would call metabolically healthy obesity.
Even in the absence of other cardiometabolic risk factors, increased fat mass and adipose tissue dysfunction contribute to a higher risk of Type 2 diabetes and cardiovascular disease. Therefore, weight management and recommendations for weight loss are still important for people living with metabolically healthy obesity.”
Other Studies Concur
Other recent research has come to the same conclusion. A prospective cohort study of 381,363 British participants, published in 2021, found that:9
“Compared with people who were not obese at baseline, those with MHO had higher incident HF [heart failure] (HR [hazard ratio] 1.60 …) and respiratory disease (HR 1.20 …). The associations of MHO were generally weaker for fatal outcomes and only significant for all-cause (HR 1.12 …) and HF mortality rates (HR 1.44 …).
However, when compared with people who were metabolically healthy without obesity, participants with MHO had higher rates of incident diabetes (HR 4.32 …), ASCVD [atherosclerotic cardiovascular disease] (HR 1.18 …), HF (HR 1.76 …), respiratory diseases (HR 1.28 …) and all-cause mortality (HR 1.22 …) …
Conclusions/interpretation: Weight management should be recommended to all people with obesity, irrespective of their metabolic status, to lower risk of diabetes, ASCVD, HF and respiratory diseases. The term ‘MHO’ should be avoided as it is misleading and different strategies for risk stratification should be explored.”
Excess Calorie Intake Is Not the Cause of Weight Gain
In the Energy Balance Podcast above, independent health researchers Jay Feldman and Mike Fave explain why eating too much and exercising too little is not the reason for weight gain. Jay is one of the best teachers of the Bioenergetic view of health. I would strongly encourage you to listen to his YouTube channel, but watch the oldest ones first so you can get grounded in the basics.
Obesity is a state of energy DEFICIENCY due to inhibited mitochondrial respiration, which causes calories to be stored as fat instead of being burned for fuel. The solution, therefore, is not to eat less and exercise more. Rather, it’s to optimize your mitochondrial function and raise your metabolic rate.
This inefficient burning of fuel (metabolizing of food) is why people who are obese typically also struggle with other health issues, such as low energy, fatigue, an inability to maintain focus, digestive problems and poor immune function.
The Bioenergetic View of Energy
As explained by Feldman, “energy,” in terms of the human body, primarily refers to your ATP level. So, ATP equals energy. The conventional view is that calories equal energy, but that’s a misconception, because calories come from three primary substrates (fat, glucose and protein), and they do not produce the same amount of ATP calorie for calorie.
Another major misconception is that when you’re gaining weight, you’re converting all your fuel (from food) into ATP and simply don’t need any more (typically because you’re not active enough), and so the excess energy is stored as body fat instead of being burned.
What actually happens is that you have a problem converting the fuel you consume into energy, so the fuel gets stored as body fat instead. In other words, you’re not producing enough energy and are in an energy-deficient state. So, it’s not excess ATP/energy that gets stored. It’s the fuel that is stored, and it’s stored because your body cannot efficiently metabolize it.
The end result is excess body fat AND insufficient energy, which in turn forces your body to downregulate other systems, such as your thyroid activity and reproductive hormones — anything that is not essential for survival.
You’re also cursed with perpetual hunger because the hunger signal is predominantly regulated by energy availability. This in turn leads to overeating, resulting in a vicious cycle of low energy and weight gain.
Decreased Energy Causes Obesity
A study10 was recently published in the International Journal of Molecular Sciences, attributing obesity to broken mitochondria. As noted by the authors:
“An important component of the pathogenesis of the metabolic syndrome is mitochondrial dysfunction, which is associated with tissue hypoxia, disruption of mitochondrial integrity, increased production of reactive oxygen species, and a decrease in ATP, leading to a chronic inflammatory state that affects tissues and organ systems.”
In the podcast, Feldman cites an earlier study, published in 2003 in the Journal of Theoretical Biology, titled “Decreased Energy Levels Can Cause and Sustain Obesity.” An excerpt from the abstract reads:11
“Current theories consider obesity a result of overeating and sedentary life style and most efforts to treat or prevent weight gain concentrate on exercise and food intake. This approach does not improve the situation as may be seen from the steep increase in the prevalence of obesity.
This encouraged us to reanalyze existing information and look for biochemical basis of obesity … We began with the contradictory information: in obesity, more calories are consumed than used up, suggesting that obese people should have excess energy.
On the other side, obese people experience fatigue and decreased physical endurance that indicates diminished energy supply in the body. The result of our work is a chain of metabolic events leading to obesity.
The crucial event is the inhibition of the TCA [tricarboxylic acid] cycle at the step of aconitase. It disturbs energy metabolism and results in ATP deficiency with simultaneous fat accumulation.
Further steps in obesity development are the consequences of diminished energy supply: inhibition of beta-oxidation, leptin resistance, increase in appetite and food intake and a decrease in physical activity.
Thus, our theory shows that obesity does not have to be caused by overeating and sedentary life-style but may be the result of the ‘obese’ change in metabolism which is forcing people to overeat and save energy to sustain metabolic functions of cells. This ‘obese’ change is caused by environmental factors that activate chronic low-grade inflammatory process in the body …”
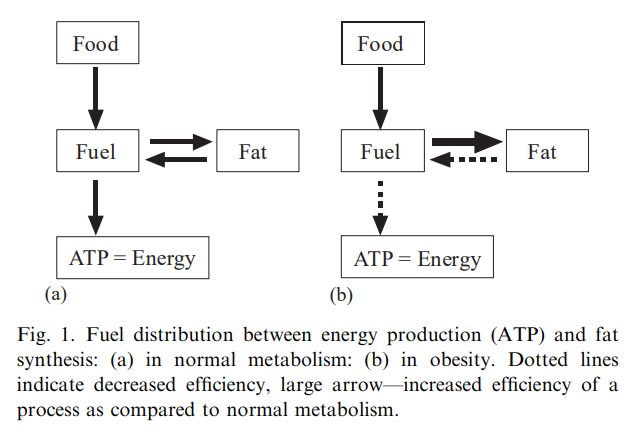
The screenshot below can be helpful. On the left is what normal metabolism looks like. The food you eat is turned into fuel, some of which is burned for energy and some of which is stored as body fat. When needed, body fat is also burned as fuel and converted into energy.
On the right is the “obese” metabolism. The primary differences here are the dotted arrows. The food consumed is turned into fuel, but very little of that fuel is converted into energy. Most of it is instead shuttled into fat storage, and because the metabolism is so inefficient, the stored fat is not released and burned for energy.
Many Normal Weight People Have Deranged Metabolism Too
As explained by Feldman, not only do obese individuals have this deranged metabolism, but many normal weight people do too. People who exercise a lot, or fast, or eat a low-carb diet may appear to have healthy metabolism because they’re not overweight, but the real reason they’re not overweight is because they’re forcing the conversion of fuel to energy through STRESS.
So, while they may not accumulate body fat, they still struggle with an energy deficiency, which can present as fatigue, brain fog, low mood, hormonal dysfunction and more.
As noted by Feldman, the bioenergetic solution to these problems is to improve the conversion of fuel to energy, “which means you have the energy available to properly function in terms of all your organ systems — your digestion, your reproductive systems, cognitive function, all of that.”
Endotoxin and PUFAs Decimate Mitochondrial Energy Production
One key strategy to optimize your mitochondrial energy production is to remove blocks in the electron transport chain so that electrons can move smoothly forward, without accumulating and backing up.
Endotoxin (lipopolysaccharide or LPS) and other bacterial toxins are among the biggest culprits when it comes to things that hinder mitochondrial energy production. These toxins can directly impair electron transport through the complexes of the electron transport chain. They can also impair certain enzymes in the Krebs cycle.
Poor digestion is frequently associated with negative gram bacteria in your gut that produce endotoxin, and this will inhibit your ability to convert food to energy, resulting in increased body fat. So, it’s important to reduce your endotoxin load. Aside from poor digestion, excess endotoxin is also a common culprit in degenerative conditions, metabolic syndrome, diabetes and fatty liver. To reduce your endotoxin load:
- Rebalance your gut microbiome by reintroducing beneficial bacteria (probiotics and prebiotics). One of the best and least expensive ways to do this is to eat a serving of fermented vegetables each day.
- Temporarily go on a low-fiber diet and avoid fiber supplements as it can feed undesirable bacteria. Avoid all vegetables temporarily and use fruit juice as your source of calories until your gut microbiome improves. Once it improves you can gradually add in whole fruits.
Once your microbiome is balanced and symptoms of poor gut function have resolved, you can slowly reintroduce starches like white rice and, if tolerated, progress to very well-cooked vegetables. Always cut back if you have signs of indigestion like belching, bloating or gas as this suggests you are not digesting those carbs yet.
Another effective blocker of mitochondrial energy production is polyunsaturated fat (PUFA). These are your processed seed oils, canola oil being among the worst of the worst. Seed oils are loaded with linoleic acid, an omega-6 PUFA, which appears to be one of the primary drivers of chronic diseases, in part due to its detrimental impact on your mitochondrial function and energy production.
So, you’ll want to severely limit your consumption of PUFAs. In addition to not cooking with them, this also means abstaining from processed foods, most of which are loaded with these harmful fats.
Rescue Remedies
While there are no magic pills to fix slow metabolism or low energy production, there are some that can help. I’ve previously written about the usefulness of niacinamide, for example. Another helpful one is methylene blue, which can both accept and donate electrons.
So, if you have blocks in the electron transport chain where most of the ATP is produced, say endotoxin or PUFAs, methylene blue can bypass those blocks, allowing your mitochondrial to produce energy anyway.
How to Gauge Your Metabolic Rate
According to the rate-of-living theory, the higher your metabolic rate — which means the quicker the electrons move from food toward oxygen, which is the final acceptor of electrons — the faster you’ll age because there’ll be higher oxidative stress.
However, deeper analysis reveals the exact opposite. The truth is, the higher your metabolic rate, the slower you age, because a high metabolism creates fewer reactive oxygen species (ROS) that can damage your tissues.
Your metabolism is high when electrons move rapidly and easily through the mitochondrial electron transport chain, which results in optimal energy production. When electrons are impeded from moving forward, they can back up, leak through the mitochondrial electron transport chain and start moving backward, where they combine with oxygen to create excessive ROS.
So, for optimal health, you want high energy production and that means a high metabolic rate. You can gauge your metabolic rate using your pulse, body temperature and calorie counting. These are not exact sciences, but can give you a general idea of where you’re at. Signs of low metabolism include:
- A body temperature below 97.8 degrees Fahrenheit upon waking, and/or 98.6 degrees F in the afternoon. You can also check your temperature before and after a meal. If your temperature drops after breakfast (compared to what it was in the morning), this could be a sign of less than optical metabolism as well.
- A resting pulse below mid-70 to low-80s, depending on your level of fitness. The greater your cardiovascular fitness, the lower your pulse rate will be, independent of your metabolic state, because your stroke volume is higher. The stroke volume is the amount of blood your heart pumps with each beat. When you’re very fit, your heart can push greater amounts of blood per beat.
- Assess how many, or how few, calories you can consume without adding to your weight. If you should be burning 3,000 calories a day, but you’re maintaining your weight on 2,200 calories a day, then your metabolism is likely low. Conversely, if you can maintain your weight when you add more calories, your metabolic rate is likely high, and the extra food will oftentimes improve your sleep, relaxation, energy and recovery.
#Obesity #Study #Fat #Fit #Myth
