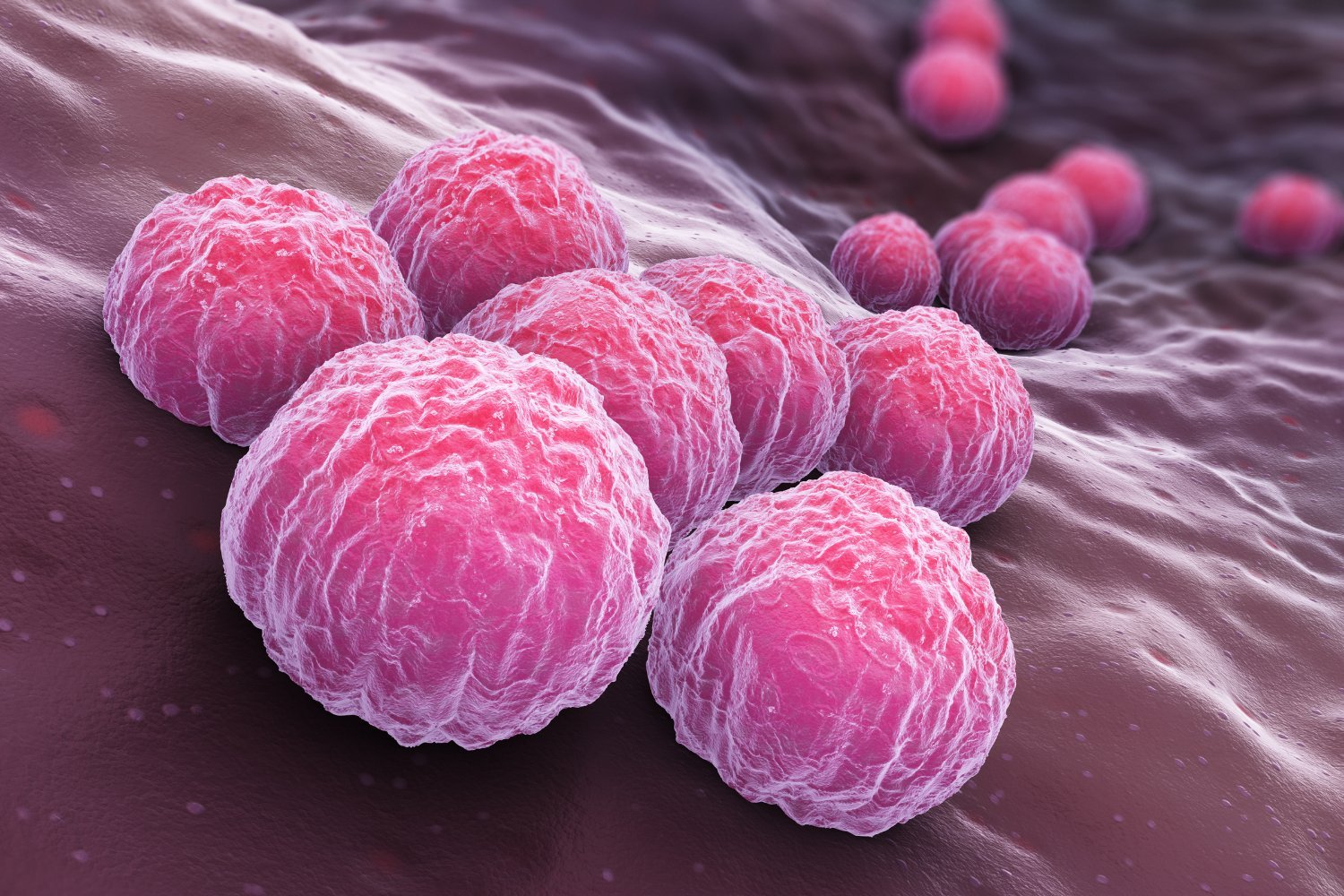
The bacteria that cause chlamydia might be trickier than we knew. In a new study this week, scientists have found evidence that these bacteria can hide in our intestines. The findings might explain why some people experience re-occurrences of chlamydia even after successful antibiotic treatment, the researchers say.
Chlamydia in humans is caused by Chlamydia trachomatis (other animals, including koalas, have their own version). It’s the most commonly reported sexually transmitted infection in the U.S., with more than 1.6 million documented cases in 2022. Though most infected people will not become sick, some will experience gruesome symptoms like bloody urination, genital discharge, or rectal pain and bleeding, depending on where the infection is located. Untreated cases of chlamydia can lead to life-changing complications like pelvic inflammatory disease, arthritis, and even infertility, while also raising the risk of catching other STIs.
Researchers at the University of Würzburg in Bavaria, Germany, led this new research, who were hoping to get to the bottom of a persistent mystery about chlamydia. Though infections remain very treatable with antibiotics (for now, at least), some people will later return to their doctors with another bout of chlamydia. When scientists have looked at these cases, they’ve sometimes found that people were reinfected by strains genetically identical or very similar to the bacteria that first infected them.
It’s possible that some of these cases come from an infection that wasn’t actually fully treated, from having sex with the same untreated partner who originally spread the infection, or from playing with a sex toy contaminated from earlier use (this is less likely since the bacteria don’t live very long outside our bodies). But some research has also suggested that chlamydia bacteria can establish a hidden reservoir elsewhere in the body, allowing them to persist and cause trouble again when conditions are right.
Other species related to C. trachomatis are known to routinely live in the guts of their hosts, hinting that our chlamydia bacteria can hide there as well. But to date, the research showing that chlamydia persistence is possible has largely been done in animals. In this new study, published this month in the journal PLOS Pathogens, the researchers say they’ve come closer to establishing that this can indeed happen in people.
The scientists grew human gut organoids—miniaturized versions of our organs or tissues—in the lab, then tested whether chlamydia bacteria could successfully infect them. The organoids were made to resemble the layers of cells that line our gut. The bacteria weren’t very good at infecting the “apical” surface, or the layer of our organs exposed to an external environment, of the organoids, the researchers found. But the bacteria could easily infect the gut organoids via the “basolateral” surface, or the layer of cells connected to other underlying tissues and structures, including blood vessels. And when the researchers looked more closely at the bacteria that infected these organoids, they spotted a familiar foe.
“In this case, we repeatedly found the persistent forms of the bacteria, which can be clearly identified with their typical shape under the electron microscope,” said lead researcher Pargev Hovhannisyan, chair of microbiology at the University of Würzburg, in a statement from the university.
The findings alone don’t provide definitive proof that chlamydia can linger in our guts, the researchers caution, so more work will have to be done to confirm and better understand this phenomenon. There are other questions left to be answered should this risk be genuine, such as how exactly chlamydia bacteria reach the gut and the specific cells they prefer to hide inside of. But whatever we learn, it shouldn’t change how sexually active people protect themselves against these bacteria. It remains important to get regularly tested for chlamydia and other STIs (at least once a year, though possibly more frequently if you have multiple partners), to consider consistently using condoms or other barrier methods, and to finish your entire course of antibiotics if you do contract chlamydia.
#Chlamydia #Hiding #Gut